Acne Treatment In Singapore
Acne vulgaris is one of the most common skin conditions in Singapore. It predominantly affects adolescents and young adults, and affects as many as 80% of teenagers in Singapore.
Commonly referred to as ‘pimples’ or ‘zits’, its associated negative impact on our physical image often leads to much psychological distress.
Although most cases of acne occur during puberty, adult-onset acne is not uncommon. Adult-onset acne is more prevalent among females, with twelve percent of women with acne at age 25 years, and five percent of women with acne at age 45 years.
Book Appointment

Managing Acne Scars
Some acne can lead to permanent scarring, such as skin depressions, deep pits, or raised areas. These scars can be improved with the following medical treatments:
- Laser resurfacing
- Fractional lasers
- TCA CROSS
- Radiofrequency microneedling
- Dermal fillers
- Steroid injections
SUCCESS CASES
*Due to MOH guidelines in Singapore, medical clinics cannot show before & after photos on their websites. However, we would be delighted to showcase our photographs and actual results during your in-clinic consultation with us.
Our Doctors
VIEW ALL
Dr. SK Tan
Special Interest
- Hyper-pigmentation
- Anti-Aging
- Acne
- Acne Scarring
- Ingredient Studies
Dr. SK Tan
Dr Tan graduated in 1971, with a Bachelors of Medicine (MB) and a Bachelors of Surgery (BS) from the University of Malaya. Dr Tan’s interest in dermatology led him to train at the St John’s Institute of Dermatology in London in the 1970s and he has since been focused in the field of aesthetic dermatology.
- MBBS
- Diploma in Venereology (University of London)
- Diploma in Dermatology (University of Wales)
- Diploma in Cosmetic Science (UK)
- Master of Business Administration
- Fellow of the American Academy of Dermatology (FAAD)
He is a member of numerous medical associations, including the American Academy of Dermatology, the International Society of Cosmetic Laser Surgeons, and the International Academy of Cosmetic Dermatology. Dr Tan was one of the first local doctors to be certified by the American Board of Anti-Aging Medicine. His personal interest in pigmentary disorders and acne has also led him to become an International Member of the Pigmentary Disorders Society of India, the Asian Society of Pigment Cell Research, and the American Acne and Rosacea Society (AARS).
Dr Tan’s work has led him to be invited to speak at numerous international conferences in the US, Europe and throughout the Asia Pacific region. He is a co-editor of “Handbook of Cosmetic Microbiology”, a reference book published by Marcel Dekker, and his papers have been published in the Journal of Cosmetic Dermatology, International Journal of Dermatology, Journal of the European Academy of Dermatology and Venereology, Journal of Cosmetic and Laser Therapy, and Expert Review of Dermatology, and has contributed a chapter in the reference book ‘Pigmentary Disorders: A Comprehensive Compendium’.
Special Interest
- Hyper-pigmentation
- Anti-Aging
- Acne
- Acne Scarring
- Ingredient Studies

Dr. Ben Yim
Special Interest
- Anti-aging
- Hyper-pigmentation
- Body-Contouring
- Fat Reduction
Dr. Ben Yim
Dr Yim graduated from Monash University in Australia with a Bachelor of Medicine and Bachelor of Surgery degree. He has also earned a Master of Science in Clinical Dermatology from the University of London and more recently in Non-Surgical Facial Aesthetics from Anglia Ruskin University in UK, as well as a Graduate Diploma in Family Physicians in National University of Singapore.
- M.B.B.S (Monash University) 1994
- Diploma Practical Dermatology (University of Wales College of Medicine) 1998
- MSc. Clinical Dermatology (University of London) 1999
- MBA (University of Chicago) 2011
- MSc Non-Surgical Facial Aesthetics (Anglia Ruskin) 2018
- GDFM (NUS) 2019
Dr Yim has been practicing aesthetic medicine in private practice since 2000. The former director of Clinical Aesthetics & Laser Centre has been offering a wide armamentarium of aesthetic services including Botulinum Toxins, fillers for facial enhancement, skin tightening, fractional lasers, threadlifts, and non-invasive body contouring treatments.
As a trainer for Allergan Medical Institute in Singapore, Dr Yim has been invited to speak and train for numerous aesthetic workshops and conferences including “The Advanced Facial Anatomy and Injectables Workshop”, Botulinum Toxins and Filler injectable training workshops organized by Allergan, “The Singapore Disease Conference 2008” and “1st International Conference on Healthcare Transformation 2008” and Forum for Professional Self-regulation jointly organized by the SingHealth Centre for Health Services Research and the NUS Medical Society, to name a few.
Dr Yim comes from a family of four doctors, all in private practice in family medicine. Despite the move into full-time aesthetic medicine, Dr Yim has also taken an interest in family medicine pursuing a Master degree in Medicine in Family Medicine in NUS in which he hopes to complete in 2020.
Outside of his profession, Dr Yim also actively participates in social projects such as tattoo laser removal for prison inmates and teenage delinquents. For leisure, he enjoys golf, reading, playing the piano and running – he has participated in several half-marathons.
Special Interest
- Anti-aging
- Hyper-pigmentation
- Body-Contouring
- Fat Reduction

Dr. Liz Lum YX
Special Interest
- Acne
- Acne Scarring
- Fillers
- Neurotoxin Injection - Botulinum Toxins
- Face Lifting
- Facial Slimming and Contouring
Dr. Liz Lum YX
Dr Liz Lum YX graduated from Trinity College in Dublin with a Bachelor of Medicine and Bachelor of Surgery degree. She has also earned a graduate diploma in aesthetic medicine with the American Academy of Aesthetic Medicine (AAAM). Apart from these, Dr Lum has also attained certification by the Ministry of Health accredited bodies under the Singapore Medical Council’s Aesthetics Dermatology Education Group for various aesthetics procedures. Before joining IDS, Dr Liz Lum YX was a surgical trainee with the hand surgery department in SGH.
- MBBCH BAO (Trinity College Dublin)
- Diploma in Aesthetic Medicine, American Academy of Aesthetic Medicine
- Accredited by the Aesthetic Practice Oversight Committee (Singapore Medical Council) for Certificates of Competence in Aesthetic Procedures
- Diploma in Cosmetic Science (UK)
Jean Cocteau once said, “If there is a defect in the soul, it cannot be corrected on the face; but if there is a defect on the face and one corrects it, it can correct a soul.”
For this reason, Dr Liz Lum YX has a special interest in acne treatment that dates back to times when she had to deal with her own acne problems and breakouts. This drove her to identify the need for innovative products and treatments to treat acne problems. She strongly believes that many acne prone patients will benefit from a combination of innovative dermatological products, lasers and medications.
Dr Liz Lum YX’s other interests include injectables such as botulinum toxins, fillers and laser treatments for pigmentary disorders. Outside of her profession, she enjoys travelling and spending quality time with her family, friends and loved ones over good meals, movies, and a cup of coffee.
Special Interest
- Acne
- Acne Scarring
- Fillers
- Neurotoxin Injection - Botulinum Toxins
- Face Lifting
- Facial Slimming and Contouring

Dr. Ian Tan
Special Interest
- Acne
- Anti-Aging
- Body Contouring
- Face Lifting
- Facial Slimming and Contouring
- Hair Regrowth
- Weight Management
Dr. Ian Tan
Dr Tan graduated from the National University of Singapore and is one of the few medical doctors selected to lead the Singapore National Healthcare Group surgical residency program. He had his basic years of training in various hospital surgical specialties and he obtained Membership of the Royal College of Surgeons of Edinburgh (General Surgery) in 2013.
- MBBS (Singapore)
- MRCS (Edinburgh)
- GDFM (Singapore)
- GDFP Dermatology (Singapore)
- Certificate in Aesthetic Medicine, Amercian Academy of Aesthetic Medicine
- Accredited by the Aesthetic Practice Oversight Committee (Singapore Medical Council) for Certificates of Competence in Aesthetic Procedures
- Diploma in Cosmetic Science (UK)
- Accredited Family Physician
- Basic Obesity Management Accreditation 2 (BOMA 2)
- Certificate Course in Andrology
Through his practice, he developed a keen clinical interest in dermatological conditions and has obtained a Diploma in Dermatology (FP) from NUS. Dr Tan aims to help his patients achieve beauty through science by using appropriate skincare, aesthetic procedures and lasers. He believes his experience in surgery will complement his work in aesthetic and dermatological procedures at the IDS clinic.
A former national, Dr Tan was an avid athlete during his college days and developed him in local and regional canoe competitions. Outside of his profession, he enjoys running and going to the gym.
Special Interest
- Acne
- Anti-Aging
- Body Contouring
- Face Lifting
- Facial Slimming and Contouring
- Hair Regrowth
- Weight Management

Dr. Michelle Wong
Special Interest
- Acne
- Acne Scarring
- Focused Ultrasound Lifting
- Skin Brightening
- Cryo based Treatment
Dr. Michelle Wong
Dr Michelle Wong graduated from The University of Melbourne, Australia with a Bachelors of Medicine, Bachelors of Surgery and Bachelors of Medical Science. She obtained her post-graduate Diploma in Clinical Dermatology with Distinction from the Queen Mary University of London, and holds a Diploma in Aesthetic Medicine with the American Academy of Aesthetic Medicine (AAAM).
- MBBS from The University of Melbourne, Australia
- Diploma in Clinical Dermatology from Queen Mary University of London
- Diploma in Aesthetics Medicine from American Academy of Aesthetic Medicine
- Diploma in Cosmetic Science (UK)
In aesthetics, Dr Wong believes she has discovered her ikigai – the intersection of what she is both good at and loves doing. Her preferred tools of the trade are injectables such as Botulinum Toxins & fillers, which she wields with finesse and intuition - often achieving what her patients desire but cannot express through words. Out of passion and interest, she regularly attends conferences and workshops, eager to learn about the latest treatments and techniques to further hone her craft.
Combining the science of medicine with the art of beauty, Dr Wong provides an honest consult to help her patients achieve their skincare and beauty goals. She believes in understated elegance – a focus on a less-is-more approach - and works to enhance her patients’ natural features whilst instilling self-confidence. Her reassuring and gentle approach puts patients at ease allowing her to achieve maximum results through safe and effective procedures.
In her free time, Dr Wong enjoys taking long walks with her dog at the park. Her family praises her inner domestic goddess that can whip up an impressive variety of home-cooked meals. She is also active in church medical missions and believes in contributing back to society through her God-given gifts and talents.
Special Interest
- Acne
- Acne Scarring
- Focused Ultrasound Lifting
- Skin Brightening
- Cryo based Treatment

Dr. Vivian Yong
Special Interest
- Acne
- Acne Scarring
- Fillers
- Neurotoxin Injection - Botulinum Toxins
- Face Lifting
- Facial Enhancement
Dr. Vivian Yong
Dr Vivian Yong graduated from National University of Singapore in 2006, and has an experience of more than 10 years in Aesthetics. She has also accumulated extensive surgical skills and experience from various rotations in general surgery, ophthalmology, and ENT.
- MBBS
- GDFM
Dr Vivian has always had a natural inclination towards science subjects and this led her into medicine. During her medical graduate days, she developed a keen interest in Aesthetics and Skincare, and she believes that Aesthetics is one area that allows her to help a patient achieve their ideal artistic expression based on science. While Dr Vivian is always keen to accommodate her patients’ needs, she ensures that their welfare remains the utmost priority. This is why Dr Vivian is loved by her patients for always being meticulous and attentive to details.
Dr Vivian’s eye for beauty goes beyond aesthetics. Outside the clinic, Dr Vivian loves to spend her time in leather crafting and jewelry making, transforming basics into beauty. She also loves spending her quiet time exercising in the gym or chilling at home with her loved one.
Special Interest
- Acne
- Acne Scarring
- Fillers
- Neurotoxin Injection - Botulinum Toxins
- Face Lifting
- Facial Enhancement

Dr. Sean Lim
Special Interest
- Acne
- Acne Scarring
- Fillers
- Neurotoxin Injection - Botulinum Toxins
- Face Lifting
- Facial Enhancement
Dr. Sean Lim
- MBBS (Singapore)
- Certified Personal Trainer
Dr Sean is a dedicated medical professional with a diverse background in procedural disciplines and holistic care. He graduated with an MBBS degree from the National University of Singapore, earning recognition on the Dean's List for his exemplary performance in his final year Professional Examination. Fully registered with the Singapore Medical Council (SMC), Dr Sean is also certified to perform aesthetic procedures by the Aesthetic Dermatology Educational Group (ADEG).
Beyond his clinical practice, Dr Sean actively engages in community service and leadership endeavours. He has contributed his medical expertise to humanitarian missions, including Naamjai Medical Missions trips to Thailand and a collaborative effort with plastic surgeons from NUH at Yangon's Defense Services General Hospital (DSGH).
Dr Sean's commitment to excellence extends beyond the medical field. As a former Singapore national athlete in pole vaulting, he has represented Singapore in numerous international competitions, earning accolades and setting records. Dr Sean’s passion for health and fitness is evident in his certification as a personal trainer and his dedication to maintaining an active lifestyle.
A proud new father, Dr Sean cherishes quality time with his family outside of work commitments, demonstrating a balanced approach to life and well-being. His belief in delivering quality care with a personal touch reflects his ethos as a compassionate healthcare provider.
Special Interest
- Acne
- Acne Scarring
- Fillers
- Neurotoxin Injection - Botulinum Toxins
- Face Lifting
- Facial Enhancement


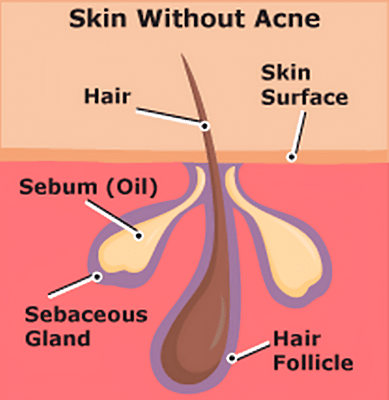
Causes of Acne
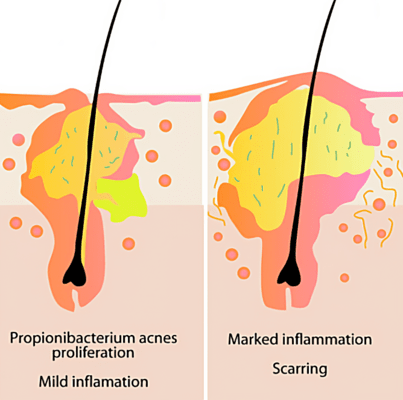
There are four main factors that lead to the development of acne.
- The presence of Cutibacterium acnes (C acnes) in the sebaceous follicle
- Androgen-mediated increase in sebum production
- Keratinocyte hyperproliferation in the follicle
- Inflammation
Other risk factors for acne include:
- Genetic factors
- Psychological stress
- Hormonal factors (eg. polycystic ovaries, puberty & pregnancy)
- Medications (eg. topical corticosteroids, anti-epileptics)
- Dairy and high glycemic index diets
Acne Treatments In Singapore
Acne Treatments In Singapore
Topical Treatments
Topical treatments are prescribed for mild acne on the face. Combinations can be used for its synergistic action. Treatment is for at least 6 months. Improvement is gradual and incremental over the 6 months. Depending on the type of acne(comedonal vs. inflammatory), our doctors will prescribe the appropriate topical treatment.
Oral Medication
When the acne condition is deemed moderate to severe, our doctors can add oral medication to the treatment. Truncal acne is usually treated with a long course of oral medication. Oral medication is usually for a period of 6 months or longer.
Oral Medication Side Effects
In-Clinic Procedures
Facial Treatments
To keep acne flares under control, regular aesthetic facial treatments may help one to manage and maintain acne outbreaks. This clarifying facial treatment combines ultrasonic deep cleansing and extractions to help clear clogged pores and comedones, along with IPL and a clay mask to calm and soothe inflamed skin.
Fractional RF Microneedling (for Acne Scars)
This non-surgical treatment uses microneedles and radiofrequency energy to stimulate collagen production and improve the appearance of acne scars. It’s commonly used to treat atrophic scars like ice-pick or boxcar scars.


What to Expect After Treatment
Acne treatment is a gradual process, and results take time. Depending on the approach whether topical, oral, or in-clinic procedures, here’s what you can typically expect:
- Gradual Improvement: Most patients begin to see clearer skin over several weeks to months. Treatment usually spans at least 3–6 months for sustained results.
- Mild Side Effects: Temporary dryness, redness, or flaking can occur, especially with topical medications or chemical peels.
- Multiple Sessions May Be Needed: In-clinic procedures like laser or light therapy often require several sessions for optimal improvement.
- Scar Management Takes Longer: Acne scar treatments such as fractional RF microneedling or laser therapy work progressively over multiple sessions.
- Ongoing Skincare Is Key: Maintenance with prescribed skincare helps prevent new breakouts and support long-term skin clarity.
Is your acne affecting your quality of life? Consult our doctors for an accurate diagnosis of your condition and a suitable treatment plan.
Book AppointmentWe treat every problem in an
efficacious way.
Step into the world of aesthetic solutions built upon medical science.Where we integrate technology, artificial intelligence and complementary skincare to address the most common skin problems.
Acne Myths
Myth: Cosmetic make-up, powder, sunscreens and dirt will block pores
Fact: Comedogenic cosmetic ingredients and products stimulate sebaceous gland activity, and lead to excess sebum production. This in turn blocks the follicles (pores) and leads to acne. It is a myth that follicles can be occluded from the exterior skin surface by cosmetic “impurities”.
Myth: Fried, spicy or oily food cause the skin to be oily and trigger acne breakouts.
Fact: Current research has not shown any correlation between consuming fried, spicy and oily food and acne. However, there is increasing evidence to show that consumption of dairy products (e.g. milk, cheese, butter) and high glycemic index food (e.g. starchy food, sugary drinks) cause acne breakouts. Whey protein consumed by athletes and bodybuilders are also associated with acne.
Myth: Only teenagers get acne.
Fact: Acne is most common in teenagers but an increasing number of adults, especially women, can get acne breakouts at any age. It has been observed that adult women aged late 30’s and early 40’s are more prone to acne.
Myth: Squeezing pimples yourself is the best way to get rid of them.
Fact: Scarring can occur even in mild cases of acne. This is due to the resultant damage to surrounding skin tissues from the inflammation. Squeezing or picking at pimples may cause more inflammation and hence more skin damage. However, the ‘pattern’ of acne scarring appears to be individual and may be genetically determined.
Myth: Getting a tan helps acne.
Fact: Some believe that getting a tan helps acne. A sunburn will only irritate the skin and lead to increased acne or cause post inflammatory hyperpigmentation(PIH) or blemishes that will take a long while to heal.
Frequently Asked Questions (FAQ)
How long does acne treatment take to work?
Most people start seeing results within 6 to 12 weeks, but full improvement often takes 3 to 6 months. In-clinic procedures and scar treatments may require multiple sessions for best results.
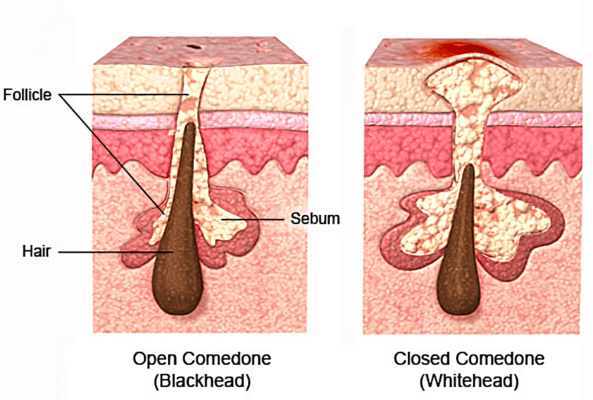
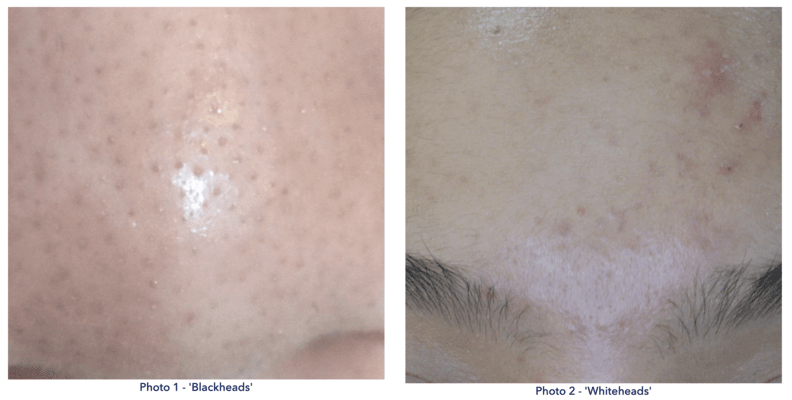
What’s the difference between acne and acne scars?
Acne refers to active breakouts such as pimples, whiteheads, or cysts. Acne scars are the lasting changes in skin texture (like pits or bumps) that may develop after the acne heals, especially if it was severe or inflamed.
Can acne treatments in Singapore be done during pregnancy?
Some acne treatments, especially oral medications may not be safe during pregnancy. However, pregnancy-safe options such as certain topical treatments or light therapies may still be used under medical guidance.
Is there any downtime after in-clinic acne treatment in Singapore?
Some treatments may cause temporary redness or mild peeling. Downtime varies depending on the procedure and individual response, and will be discussed during consultation.
Can acne be permanently cured?
While acne can be well-controlled with treatment, it may recur if underlying factors (like hormones or stress) persist. Long-term management and personalised care help reduce breakouts and minimise flare-ups.